Universal health coverage and well-being for all
It’s too early to determine the full implications of Covid-19 on world health yet, but it’s impacting and overwhelming health systems globally. Prior to the coronavirus pandemic, even though improvements had been made for millions, less than half the world’s people were covered by essential health services (UN, 2017), with 100 million pushed into extreme poverty, forced to survive on just $1.90 or less a day, because of having to pay for health services out of their own pockets (World Health Organisation, 2018). Tourism can help.
For this reason, Sustainable Development Goal #3 of the 17 Global Goals is:
SDG #3 “Ensure healthy lives and promote well-being for all at all ages"
The Goal addresses all major health priorities, including reproductive, maternal and child health; sexual health; communicable (passed from person to person), non-communicable and environmental diseases; and mental health. It calls for Universal Health Coverage, access for all to safe, effective, quality and affordable medicines and vaccines, more research and development, increased health financing, and strengthened capacity of all countries in health risk reduction and management.
Universal Health Coverage
UHC is key to people’s and nations’ health and well-being, and the World Health Organisation’s number one goal. It's about ensuring all people can get quality health services, where and when they need them, without suffering financial hardship and without having to choose between good health and other life necessities. Universal means for all, without discrimination, leaving no one behind. Everyone everywhere has a right to benefit from health services they need without falling into poverty when using them.
Currently, as well as millions of people still with no access at all to health care, millions more are forced to choose between ‘catastrophic expenses’ on health care and other daily expenses such as food, clothing and even a home.
National health systems are often under-resourced, private healthcare prohibitively expensive, and affordable services extremely limited, leaving many with no viable healthcare options. Risk reduction strategies are therefore vital to reduce the need for medical care.
Quality, accessible primary health care is the foundation for universal health coverage and we must do more to improve the quality and safety of health services globally: Unsafe and low-quality health care ruins lives and costs the world trillions of dollars every year. At its heart, primary health care is about caring for people and helping them improve their health or maintain their well-being, rather than just treating a single disease or condition.
Health is a political choice. Experience shows that universal health coverage happens when political will is strong and robust financing structures key. More investment in primary health care is needed to make universal health coverage a reality. Countries that invest in UHC make a sound investment in their 'human capital' (WHO), not only enhancing people’s health and life expectancy, but also protecting countries from epidemics, reducing poverty and the risk of hunger, creating jobs, driving economic growth and enhancing gender equality.
To meet the health workforce requirements of the Sustainable Development Goals and universal health coverage targets, over 18 million additional health workers are needed by 2030, especially in low- and lower-middle-income countries. Investments are needed from public and private sectors in health worker education, and in the creation and filling of funded positions in the health sector and health economy.
Progress on Sustainable Development Goal 3 Good Health & Well-Being
2.5 billion-3.7 billion: The number of people covered by Universal Health (2017): just 30-50% of global population.
Only 12-27% of the population in low-income countries were fully covered that year.39-63%: of the global population will be covered vs target for full Universal Health coverage by 2030 If current trends continue.
12.7% (927 million people): The number of global population spending more than 10% of household budget on health services, rising from 9.4% (2000-2015).
400 million+ people: have no basic healthcare, and 40% lack social protection (UNDP).
1.6 billion+ people live in fragile settings where protracted crises, combined with weak national capacity to deliver basic health services, present a significant challenge to global health.
Every 2 seconds: Someone aged 30-70 dies prematurely from non-communicable diseases: progress is slow on the 71% of all worldwide deaths attributable; 85% of the 15 million premature deaths (before age 70) in low- and middle-income countries.
7 million people die every year from exposure to fine particles in polluted air.
1/3 people globally living with HIV are able access antiretroviral therapy (UN, 2019).
One of every three+ women have experienced either physical or sexual violence at some point in their life resulting in both short- and long-term consequences for their physical, mental, and sexual and reproductive health.
38%: The drop in maternal mortality 2000-2017, from 342 deaths to 211 deaths per 100,000 live births worldwide. But this is less than half of the 6.4% annual rate needed to achieve the global target by 2030.
6.2 million (est) children and adolescents under the age of 15 years died in 2018, mostly from preventable causes (WHO).
5 million+ children die even before their fifth birthday every year still, many in places we visit: 4/5 in sub-Saharan Africa.
16,000 children die each day from preventable diseases such as measles and tuberculosis and AIDS, now the leading cause of death among teenagers in sub-Saharan Africa and second globally (UN): deaths avoidable through prevention, treatment & education.
45% of deaths in children under 5 relate to nutrition factors. Malnourished children, particularly those with severe acute malnutrition, have a higher risk of death from common childhood illness such as diarrhoea, pneumonia, and malaria.
The Impact of Covid on SDG 3 Good Health & Well-Being
We need to get one billion more people to benefit from Universal Health Coverage by 2023 if we are to meet the Sustainable Development Goals by 2030. But Covid 19 has disrupted and suspended other health services, and if current trends continue, only 39-63% of the global population will be covered by such services by 2030. Income loss due to Covid and subsequent recession will exacerbate the situation which has already seen decades of improvements reversing:
An estimated 1 billion people will spend at least 10% of household budget on health care in 2020, most in lower-middle income countries. Covid exacerbates the situation with potential expenditure increases and income reductions.
Childhood immunisation programmes have been interrupted in 53% of the 129 countries where data are available.
At least 24 million people in 21 lower-income countries are at risk of missing out on vaccines against polio, measles, typhoid, yellow fever, cholera, rotavirus, human papillomavirus (HPV), meningitis A and rubella.
118 low- and middle-income countries could see an increase of 9.8 to 44.8% in under-5 deaths per month and an increase of 8.3% to 38.6% rise in maternal deaths per month, over a period of six months.
Fears of contracting Covid combined with disruption to global supply of contraceptives and family planning services could see millions of unintended pregnancies. Globally, more than 250 million women have an unmet demand for modern contraceptives (UN Stats).
People with pre-existing non-communicable diseases are more vulnerable to becoming severely ill with Covid19, but prevention and treatment services have been severely disrupted since the pandemic began, with low-income countries most affected.
Covid19 disruption has inflated the number of people not receiving the health services and medicines they need. Covid could cause a spike in illness and deaths from other communicable diseases eg. Aids, Malaria & TB.
Covid is highlighting the existing shortage of health professionals in many countries, particularly in regions with highest disease levels.
The need for greater public health preparedness and support has never been clearer but huge disparities in countries’ abilities to cope with and recover from the COVID-19 crisis. Official development assistance (ODA) plays a vital role, but faces cuts due to Covid.
Challenges of SDG3, Health & Well-Being
Poor health was recognised by the government in Madagascar as one of the key challenges in the Madagascar Action Plan of 2007-2012, but since 2009, political crisis saw government spending on health cut by 75%, education cut by 82%, the price of basic food staples like rice double, and the value of saleable assets like cattle halved. As such, Madagascar is one of the world's least developed countries and most impoverished.
“At only $22 per day, the Malagasy national health system is amongst the worst funded in the world” — World Health Organisation, 2014.
SEED Madagascar volunteers work on grassroots projects alongside Malagasy communities and their own sustainable solutions for health, education, livelihoods and conservation in this amazing destination.
Malawi is also amongst the world's least-developed and lowest per capita income countries in the world, heavily dependent on outside aid to meet needs for healthcare. RSC seek to rectify this through sustainable development by social enterprise, reducing the dependence on the aid industry by driving tourism-generated income to rural communities through partnership and education.
In Kenya, MWCT supports the Maasai with employment of the only doctor and provision of the only ambulance in the area; 4 sustainably solar-powered health facilities with dispensaries and one clinic equipped with modern laboratory for enhanced diagnosis and treatment, a lab technician and 7 support staff.
Jicaro Island Ecolodge’s initiatives have included creating a new community health centre, enabling medical professionals to operate vital equipment needed for medical examinations.
Tiger Mountain Pokhara Lodge in Nepal provide an ambulance for emergencies and have supported the local Nepal Red Cross branch to construct a meeting hall as a training and disaster-preparedness centre.
Child Health
Great strides have been made:
The global under-5 mortality rate fell from 76 deaths per 1,000 live births in 2000 to 42 in 2015, and to 39 in 2018.
The global neonatal mortality rate fell from 31 deaths per 1,000 live births in 2000 to 18 deaths per 1,000 in 2018.
By 2018, 121 countries had already met the SDG target on under-5 mortality, and 21 countries are expected to do so by 2030. However, progress will need to accelerate in 53 countries, two thirds of which are in sub-Saharan Africa.
Despite progress, 5.3 million children died before reaching their 5th birthday in 2018 alone; almost half of those deaths, 2.5 million, occurred within the first 28 days of life (the neonatal period).
Sub-Saharan Africa remains the region with the highest under-5 mortality rate: in 2018, 1 in 13 children died before reaching age 5, that is 16 times higher than the average in high-income countries.
Children born into poverty are almost twice as likely to die before the age of five as those from wealthier families. And children of educated mothers - even mothers with only primary schooling—are more likely to survive than children of mothers with no education.
In Madagascar, inadequate diets lead to 50% of children under 3 malnourished and suffering retarded growth, with 10% dying (40% in rural areas) before the age of 5 from easily preventable diseases, such as diarrhoea.
In Kenya, MWCT’s health outreach to remote areas has meant greater child immunisation, prenatal care, early disease detection and treatment including for breast and cervical cancers.
In Nicaragua, Jicaro Island Ecolodge aim to fight malnutrition with “a glass of milk” (the project’s name) and a snack before classes for students.
In South Africa, Grootbos Foundation supports early learning centers and a food scheme across its daily multi-sports training programme, reaching the lives and providing tens of thousands of meals to thousands of children.
Maternal Health
Whilst maternal mortality has declined significantly, every day hundreds still die during pregnancy or from child birth-related complications.
Maternal mortality ratio fell by 38% 2000-2017, from 342 deaths to 211 deaths per 100,000 live births worldwide. On average, 2.9% pa. But this is less than half of the 6.4% annual rate needed to achieve the target of 70 maternal deaths per 100,000 live births by 2030.
Every day in 2017, approximately 810 women died from preventable causes related to pregnancy and childbirth.
Sub-Saharan Africa and Southern Asia account for about 86% of maternal deaths globally.
94% of all maternal deaths occur in low and lower middle-income countries. (Unicef).
Only 60% of all births in sub-Saharan Africa and 77% in Southern Asia were assisted by skilled professionals (2014-2019, UN Stats).
With 15% rise in births expected 2019-2030, an estimated 17 million in sub-Saharan Africa will have no skilled professional attending.
In developing regions, where only half of women receive the recommended amount of health care they need, the maternal mortality ratio – the proportion of mothers that do not survive childbirth versus those who do – is 14 times higher than in developed regions.
Young adolescents (ages 10-14) face a higher risk of complications and death as a result of pregnancy than other women (unicef).
In Madagascar, Malagasy women are over 55 times more likely to die from maternity related causes than women in the UK. Increasing community awareness of healthy practices during pregnancy and birth can be offered through education of pregnant women, their families and community elders. This may include simple messages such as the importance of good nutrition during pregnancy, reinforced through illustrated information cards specifically designed for people who cannot read or write, and home visits.
SEED Madagascar’s health education project in Fort Dauphin increases women’s access to quality sexual, reproductive, maternal and child health information.
In Kenya, MWCT was donated an ambulance in 2012 which is a huge help and has expanded the reach of medical capabilities for emergencies in remote villages. For example, for local Maasai in Kuku Group Ranch, enabling emergency c-sections to be performed where otherwise a mother or baby's life could in jeopardy.
Sexual Health
Expanding access to modern contraceptives is essential to ensuring universal access to sexual and reproductive health-care services.
Sexual health is often taboo in traditional societies, but high incidence of Sexually Transmitted Infections (STIs) can suggest widespread practice of risk-taking sexual behaviours and high vulnerability to HIV. STIs are unpleasant and embarrassing at the best of times, no one likes having to go and get tested. However, they are a serious health hazard and can increase the chances of contracting HIV, if exposed through sexual contact, by as much as 200%-500%. So, no matter how embarrassing or awkward to discuss testing with a partner, STIs must be taken seriously and action taken as soon as possible. Without having the correct knowledge, people are prevented from openly discussing sexual health matters and the ability to act on it, so STIs and HIV/AIDS will continue to spread. Education is key.
HIV & AIDS
Advances have been negligible since 2015, putting the world off track in achieving the SDG target. That said, globally (UNAIDS):
Globally, about 7 in 10 adolescent girls and women 15–24 years old do not have knowledge of HIV (UNAIDS, 2018).
38 million people globally were living with HIV in 2019 but just 25.4 million people accessing antiretroviral therapy (UN).
1.7 million people became newly infected with HIV in 2019.
690 000 people died from AIDS-related illnesses in 2019.
75.7 million have become infected with HIV and 32.7 million have died from AIDS-related illnesses since the start of the epidemic.
Tuberculosis remains the leading cause of death among people living with HIV, around one in three AIDS-related deaths.
Adolescent girls and young women face gender-based inequalities, exclusion, discrimination and violence, putting them at increased risk of acquiring HIV.
HIV is the leading cause of death for women of reproductive age worldwide.
AIDS is now the leading cause of death among adolescents (aged 10–19) in Africa and the second most common cause of death among adolescents globally.
A 6-month complete disruption in HIV services due to Covid, including antiretroviral therapy, could lead to more than 500,000 additional deaths in 2020–2021 in sub-Saharan Africa from AIDS-related illnesses, including tuberculosis.
The epidemic varies considerably between countries and regions. Africa remains most severely affected, with nearly 1 in every 25 adults (4.1%) living with HIV and accounting for nearly two-thirds of the people living with HIV worldwide (WHO, 2018).
HIV and poverty go hand in hand: Poverty both increases vulnerability to HIV infection, and households affected by HIV are more vulnerable to falling into and remaining in poverty. Poverty-induced hunger leads to a lack of nutrition, and lack of universal health coverage restricts access to HIV prevention and treatment. HIV-related illness impedes school attendance and learning, as does stigma and discrimination, leading to yet lower access to health care and housing. People living with HIV experience unemployment rates three times higher than national unemployment rates. It’s a vicious circle.
Malawi’s high prevalence of HIV/AIDS (12% of the population), sees at least 70% of Malawi's hospital beds occupied by HIV/AIDS patients.
In contrast, economic empowerment, safe and secure working and learning environments, social protection and nutritional support can reduce poverty and HIV vulnerability and help keep people with HIV healthy. High-quality education, including on sexual and reproductive health, can empower young people and provide life skills for responsible and informed sexual and reproductive health decisions.
So whilst young people are particularly at risk, they are also quick to pick up new information and more open and willing to change their behaviour than older people. A broad sexual health education can offer the people tools necessary to negotiate safer sexual relationships with the goal of preventing the transmission of HIV and STIs and reducing unintended pregnancies, safe sex, and raising awareness for STIs and HIV. Taking control of sexual health and making healthier life decisions can impact on future generations.
SEED Madagascar works with young people to raise awareness of safe sexual practices and develop their sexual health knowledge prior to the establishment of sexual practices, which can be as young as 11 in the region, encouraging people to change behaviours.
In Kenya, MWCT hold regular friendly youth sports tournaments to encourage health education, promotion, awareness and counselling including for Female Genital Mutilation (FGV) and HIV/Aids, including voluntary testing.
Tuberculosis (TB)
Tuberculosis is the world’s top killer from a single infectious agent and the tenth leading cause of death overall.
The current pace of progress is not fast enough to meet the SDG target of ending the epidemic by 2030.
If the COVID-19 pandemic leads to a 25% global reduction in expected tuberculosis detection for 3 months given disruptions, then a 13% rise in tuberculosis deaths could be expected, bringing the world back to the mortality levels of 2015.
Malaria
After years of impressive reductions in cases of malaria, progress has stalled, which may lead to the world failing to achieve the SDG target of ending malaria. Due to Covid, cancellation of prevention campaigns and severe disruptions in treatment means that the projected malaria deaths in sub-Saharan Africa alone could exceed the number of global malaria deaths in 2000, when the malaria epidemic was at its peak.
Sub-Saharan Africa could see a 23% increase in cases and a 100% increase in deaths by the end of 2020 (versus 2018 baseline).
Sanitation & Hygiene
Covid19 has reminded us of the importance of handwashing. Handwashing with soap can also slow down the spread of Ebola, reduce the likelihood of contracting blinding trachoma and prevent life-threatening illnesses such as diarrhoeal diseases, cholera, pneumonia and intestinal worms.
In 2012, an estimated 889,000 people died from infectious diseases caused largely by faecal contamination of water and soil and by inadequate hand-washing facilities and practices resulting from poor or non-existent sanitation services, with household and ambient air pollution resulting in some 6.5 million deaths.
In 2016, one in four health-care facilities worldwide lacked basic water services, affecting more than 2 billion people and increasing the infection risk of people seeking medical care, and one third of all primary schools lacked basic drinking water, sanitation and hygiene services, affecting children’s health, education and future livelihoods, particularly girls coping with menstruation.
In 2017, 60% people worldwide and only 38% in least developed countries had a basic handwashing facility with soap and water at home, leaving an estimated 3 billion people without. The proportion lacking a basic sanitation service decreased 27%, yet 701 million people still practiced open defecation. 1.8 billion people use a drinking water source that could be contaminated with faeces (UN, 2019).
In Malawi, 2 million don't have access to safe water; 10 million don't have access to adequate sanitation and over 3,000 children die every year from diarrhoea caused by unsafe water and poor sanitation.
Travel to Malawi and your costs include a contribution to local projects including health. On many of the trips, you can learn about village healthcare provision, clean water access HIV, malaria, bilharzia and malnutrition, work with a community NGO and volunteer to raise awareness of a key rural health issues.
Open defecation occurs where people have no choice but to defecate outside onto the ground, often in full view of other people. It affects around 15% of the world’s population, almost entirely in poor areas. It’s unpleasant to live with and bad for public health – attracting flies and pests which transfer germs from exposed faeces to food and water sources and spread disease. A single gram of faeces can contain as many as 10,000,000 viruses, 1,000,000 bacteria, 100 parasitic cysts and 100 parasitic eggs. However, a lack of material resources coupled with local taboos can make this no simple challenge.
In Madagascar, poor hygiene leads to typhoid, polio, acute respiratory infections and trachoma blindness. Only 14% of people have access to improved sanitation facilities (Unicef, 2014).
SEED Madagascar is tackling open defecation through projects in urban Fort Dauphin and rural communities to stimulate debate around the issue, encouraging people to question traditional practices and to adopt new, healthier approaches, supported by the construction of hundreds of new latrines built in homes and schools throughout the region. Some 38,000 people (60% of Fort Dauphin’s population) are expected to participate in at least one of the project’s activities and the entire population will benefit from a cleaner, safer environment.
Non-communicable Diseases (not passed from person to person)
Of all deaths among people under the age of 70, (referred to as ‘premature deaths’), 52% are from non-communicable diseases. Of those, over 75% are caused by the four main categories of non-communicable disease: cardiovascular disease, cancer, diabetes and chronic respiratory disease. Every 2 seconds someone aged 30-70 years dies prematurely from non-communicable diseases.
Respiratory disease is a common consequence of smoke inhalation caused by fossil fuel fires.
SEED Madagascar is supporting people to build fuel-efficient stoves to minimise smoke inhalation and eye infections as well as reduce pressure on protected forests.
Substance use and substance-use disorders have also created a significant public health burden.
Worldwide, alcohol consumption was highest in the developed regions (10.4l per person) and lowest in Northern Africa (0.5l per person).
In 2013, only about 1 in 6 people worldwide suffering from drug-use disorders received treatment: Approximately 1 in 18 in Africa, compared with 1 in 5 in Western and Central Europe.
Mental health disorders such as anxiety and depression occur in all regions and cultures and can lead to suicide: 86% under the age of 70, and globally, the second leading cause of death age 15-29.
Plastic pollution
”It is high time we turn our attention fully to one of the most pressing problems of today – averting the plastic pollution crisis – not only for the health of our planet, but for the wellbeing of people around the world.” - Sir David Attenborough
These are words in #Attenborough's forward in “No Time To Waste”, the first report to highlight the impacts of plastic pollution not just on precious species and natural places but also on the world’s poorest people. The report was produced by the Tearfund development agency, conservation charity Fauna & Flora International and waste management charity WasteAid.
As our ability to produce and use plastic on an industrial scale far outstrips our ability to manage it, plastic chokes up our rivers and seas, and we ship it for payment to poorer countries, where it is causes serious illness and death. Every 30 seconds, 30 double-decker busloads of plastics are burned or dumped in developing countries, causing up to a million deaths a year from diseases caused by mismanaged waste.
According to the World Health Organization (WHO), rain collecting in plastic packaging is a ‘notorious’ breeding ground, with mosquitos flies and rats, then spreading malaria and dengue fever.
Combined with poor sanitation, people living near rubbish-build-ups are twice as likely to get killer diarrhoea-causing diseases like cholera.
The burning of plastic is also thought to cause a fifth of deaths from air pollution, which kills an estimated 3.7 million people a year, causing heart disease and cancer from the tiny particles such as black carbon, mercury and polychlorinated biphenyls compounds released into the air. Children from slums in Ethiopia with uncollected waste have been found to be six times more likely to suffer acute respiratory infections.
It is also damaging farming as goats and cows eat plastic waste, as do wildlife such as albatross and whales, often suffocating or clogging their stomachs and starving to death.
This ‘throwaway culture’ of the west, half of plastic used only once before being discarded, the shipping of our spoils, and the fact that globally two billion people, 25%, don’t have their rubbish collected, is all contributing to this problem.
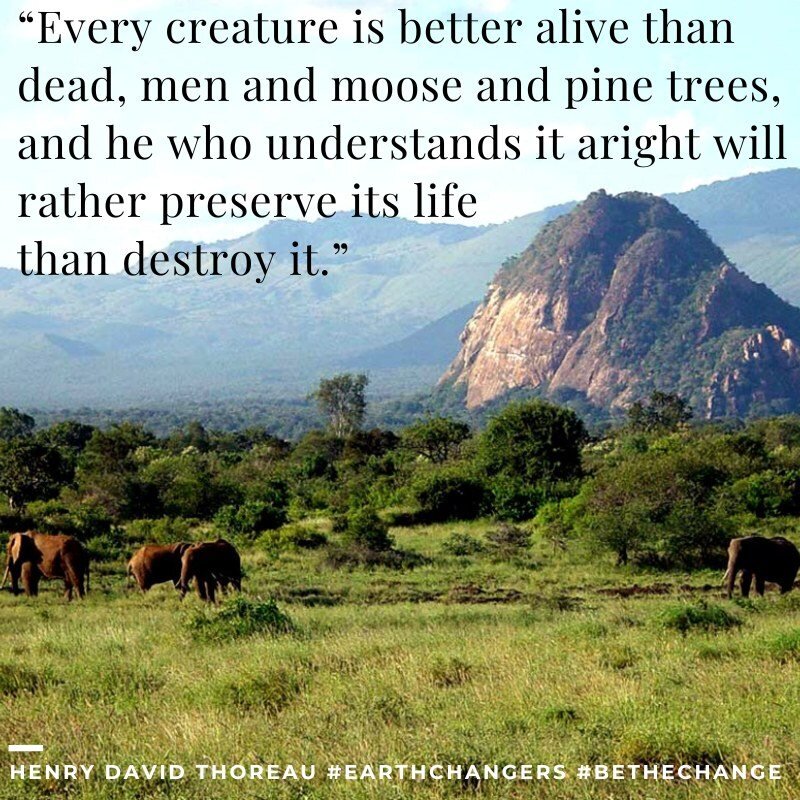
Planetary Health
An emerging discipline, planetary health looks at the links between human and ecosystem health, including zoonotic diseases such as Ebola and Covid19. Whilst nature and ecosystems pose threats, the health risks in a natural environment can be made much worse by humans. Environmental changes including development that erodes biodiversity influence the probability that humans will be exposed to infectious diseases and transmission of pathogens. Demand for wood, minerals, agriculture and meat leads to degraded landscapes and ecological disruption that drives disease. Our destruction of nature is creating the destruction of our health.
Healthy Lifestyles
Take a trip to one of our fantastic destinations and you’ll be supporting their local communities and their wellness initiatives, and not just in their physical health. Healthy activities and sport also play a key role in mental health and attitudes, bringing people together for support and personal development.
“Sport has the power to change the world. It has the power to inspire, it has the power to unite people in a way that little else does. It speaks to youth in a language they understand. Sport can create hope, where once there was only despair. It is more powerful than governments in breaking down racial barriers. It laughs in the face of all types of discrimination.”
In Kenya, MWCT hold regular friendly youth sports tournaments to encourage health education, promotion, awareness and counseling including for Female Genital Mutilation (FGV) and HIV/Aids.
Nikoi Island organised the first children’s sports program on the island of Bintan, their Foundation provides coaching staff, equipment (sold through a village shop on buy back scheme) and ground maintenance.
Our Own Health
To be able to support others, we must not forget our own health.
The accessibility of international flights has been blamed as skin cancer rates have soared overall by 45% in a decade in the UK, especially in men (55% increase) and the under 50s (70% increase). The sun is the primary cause and skin damage in earlier years can permanently increase cancer risk (The Independent, 2018). But a tan is not a sign of good health, rather it is your body trying to protect itself, and as many as 90% skin cancer cases could be prevented by using simple skin protection.
We can also make lifestyle choices in our own consumption and exercise, which can affect the health of communities half the world away (such as reducing all use of plastics) and in taking breaks for our all-round well-being.
We need to get away from work and daily life, to switch off our stressors, breath in fresh air, relax, retreat and recharge. Spending time in nature is energising, connecting with people is motivating and exercise is revitalising, and can support community health projects, such as our partners’:
Detox with organic, local food with out of this world taste; de-stress and be pampered with a spa; retreat, relax and recharge in a hammock in Costa Rica, Nicaragua or Indonesia.
Switch off from your usual world and into incredible nature in the amazing Galapagos Islands or Kenya.
Avoid the temptation and digital detox on Nikoi Island and Chumbe Island.
Improve your fitness with a charity challenge in Malawi, horse-riding in Kenya, snorkelling at Chumbe Island Marine Park in Tanzania and all activities at Nikoi!
Unwind with yoga in Costa Rica, Nicaragua and Kenya.
Enjoy the freedom of the frontier on horseback off the beaten track in Croatia.
And often, change is as good as rest: join a sailing expedition across the ocean for a real change of scene.
Discover true health and wellness with all of our Earth Changers Places!
Links with the other Sustainable Development Goals
Goal 1 - End Poverty: There is a correlation between income inequality and higher rates of health problems (eg. obesity, mental health),
Goal 2 - Zero Hunger: Without enough of the right nutrition, malnutrition results in bad health and disease in a vicious cycle.
Goal 4 - Education: Training of medical professionals and consumer understanding is essential for effective health systems and risks.
Goal 5 - Gender Equality: Globally, women face gender-based inequalities, putting them at increased risk of HIV, violence and death.
Goal 6 - Clean Water & Sanitation: is quite simply a prerequisite for health. Lack of water or sanitation spreads disease.
Goal 7 - Sustainable Energy: is required for health services & infrastructure; health and energy access vulnerability often go together.
Goal 8 - Decent Work & Economic Growth: Ill health prevents people working, costing personal livelihoods and local economy.
Goal 10 - Equality & Reducing Inequalities: High inequality plays out in large disparities in access to health care and services.
Goal 11 - Sustainable Cities & Communities: Slums have high rates of unsanitary conditions, disease and lack basic health care.
Goal 12 - Sustainable Consumption & Production will help provide nutrition and eliminate toxic pollutants and support health.
Goal 13 - Climate Change: affects agriculture and creates food insecurity leading to malnutrition, ill health and high mortality.
Goal 14 - Life Under Water: The marine environment is a vital source of protein for diets and fresh air for well-being breaks.
Goal 16 - Peace, Justice & Strong Institutions: Exclusion, injustice and conflict lead to sexual exploitation, ill health, stress and injury.
Goal 17 - Partnerships: Multi-stakeholder partnerships can step in where public funds are not available to support health initiatives
Next SDG4: Quality Education >
< Zero Hunger SDG2: Previous